Theory Versus Practice in Here Be Dust
- May 21, 2017, 12:32 p.m.
- |
- Public
As the saying goes, “No news is good news,” which is why I haven’t written here for a while. I still have good news, but it took some twists and turns and more than a bit of nervousness to get there.
On April 11 I was at my desk, minding my own business, when I was whammed by fatigue. As in: I needed to lie down before I fell down. The last time I had felt this way was when I was undergoing chemo – or, to be more exact, getting Adriamycin/Cytoxan chemo, because Taxol had never hit me like this.
I was scheduled for my regular three-month oncology checkup ten days later. I told myself: Let’s see what happens and raise this with the oncologist.
A week later I was calling my PCP instead. I could barely remain upright. Even after a full night’s sleep I awoke exhausted. My eyes felt as though they were burning and the skin on my face felt too tight, as though it would crackle at a moment’s notice. It all felt very flu-like, but my temperature was normal. By and large my days consisted of: wake up, have some food, nap, repeat. I did manage to work out, but at considerably reduced intensity. Doing errands felt like sleepwalking.
When I was getting A/C, that debilitating fatigue generally lasted for two days, three at most, following each infusion and once my steroid had worn off. Now, out of the blue, that same kind of fatigue was lasting for a solid week.
I wondered if my TSH (thyroid hormone) might be involved, because it had been elevated the month before. But it had also been elevated (and even more so) in August 2015, without this kind of fatigue.
My PCP took me as a walk-in about an hour after I called her. After establishing that nothing else was going on (including giving me an EKG, which was normal – heart disease runs in my family), she offered to give me a B-12 shot. I took it.
The next day I felt considerably better. The day after that I was just about back to “normal” (that is, my “new normal” after cancer treatment). I subsequently received three more B-12 shots, spaced a week apart, and will get my next shot four weeks after the previous one. I also have a lab requisition to get my TSH retested, just in case.
I saw my oncologist three days after my PCP and told him about the fatigue. He seemed satisfied that it had lifted following the B-12 shot and told me that such fatigue can happen with anastrazole. By this time I had been taking anastrazole (to fight against cancer recurrence) for about 2-1/2 years, so I was a bit skeptical. Why would I feel that effect now, after all that time?
However, his statement was validated at my breast cancer support group, which met on the heels of my appointment. Three other members, all taking anastrazole, reported the same thing. Two swore by B-12 shots. The third now plans to start getting B-12 shots.
My oncology checkup had gone pretty much as expected. CBC (complete blood count) results came back almost instantly, with a couple of outliers related to immunity but no cause for concern. CMP (complete metabolic profile) results would follow in a few days, and then my cancer marker results.
The following week my oncologist’s assistant left a fairly nonspecific message on my machine. I logged onto my patient portal and then reached for my phone. When the assistant answered, I said, “I know why you called.”
My oncologist tests for three cancer markers: CEA, CA 15-3, and CA 27-29. That last marker, which had been rising steadily throughout the past year, had crossed into the High range. He wanted to retest.
Cancer markers are not considered to be reliable indicators. “In breast cancer care, three tumor markers – cancer antigen 15-3 (CA 15-3), cancer antigen 27.29 (CA 27.29), and carcinoembryonic antigen (CEA) – have been used to help monitor metastatic breast cancer (advanced disease), but they have not been found to be useful to find a breast cancer recurrence or lengthen lives in patients who had early-stage breast cancer and who are now disease-free,” according to the American Society of Clinical Oncology. “These tests often lead to over-treatment and wrong diagnoses, including increased anxiety, which significantly harm a person’s quality of life.” ASCO does not recommend testing cancer markers in people like me, who were treated for early-stage breast cancer “with curative intent” and who are asymptomatic.
Breastcancer.org concurs: “While breast cancer blood marker tests are promising, they’re not absolutely conclusive. When a breast cancer blood marker test comes back negative, it doesn’t necessarily mean you’re free and clear of breast cancer. And a positive result doesn’t always mean that the cancer is growing.”
At the same time, many oncologists still order cancer markers for early-stage breast cancer patients, going against the guidelines. This is due in large part to patient demand. In my case, it’s due to my oncologist’s preference. I have questioned his testing of my markers in the past. His reply was that other than mammograms, the markers are now the only things he has to go by.
Now I faced the uncertainty that came with a high marker following a year-long, upward trend. The trend in particular was concerning. Also concerning, for a much different reason, was the need to get more blood work done, because my tiny veins make me a hard stick.
The oncologist’s assistant told me of another patient, also a hard stick, who swears by pineapple juice. No amount of water drinking had worked for him. So, in addition to plenty of water, the man drank a liter of pineapple juice an hour before blood work and voila! I tried doing the same for my marker retest and had the easiest blood draw in at least a year. The phlebotomist said my veins were standing right up. Success w/one stick! Alas, I can’t use the technique for fasting tests, but I’ll manage.
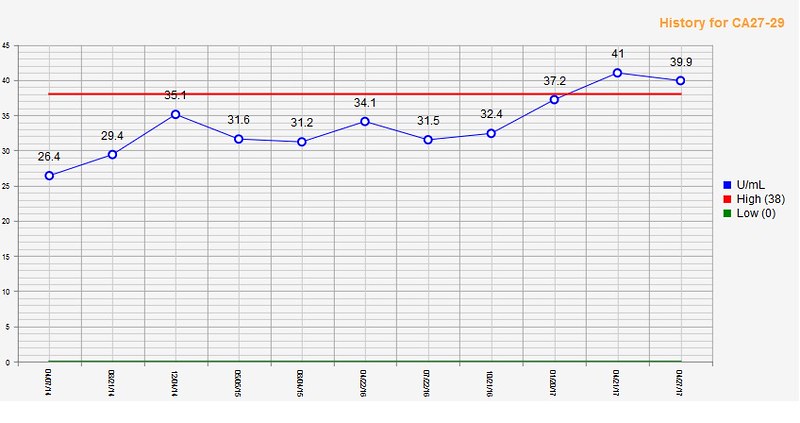
The marker retest showed a very slight drop, but the reading was still high. My oncologist ordered a PET scan.
(I asked his assistant whether any connection could be drawn between the high readings, my elevated TSH, my fatigue, or the B-12 shots. He said there wasn’t enough research done to say anything one way or the other.)
Art formed part of my meditation during all this. “World Enough and Time” is a manipulation of one of my mammogram images, plus a star stencil created by Stefano Fiore.
One month to the day after my severe fatigue had set in, I had my PET scan.
The following day I saw the result on my patient portal: “No hypermetabolic malignancy/metastases.”
Whew!
My oncologist saw me the following week to go over the results, and I came with questions. First, I asked him, “In your experience, how often do you see this sort of thing, where a marker’s been climbing over time and it passes into the high range, but the PET scan is still normal?”
“I see that quite a few times,” he said. “The marker goes up, but we are obliged to do the test because there are people where the marker goes up and the PET comes back positive. There’s no way for us to ignore. I don’t use the marker with a new patient as a diagnosis. But once I have established diagnosis, we use the markers as a follow up.”
I said, “From my understanding, one of the reasons why things like marker tests and PET scans are not recommended for people who are early stagers and treated with curative intent, who are asymptomatic … I think even if a PET shows something, there’s no difference in overall survival found. But I don’t see anything talking about disease-free survival.”
He said, “The problem with the overall survival thing is, there are not enough studies. Because some people don’t show for many, many years, and the studies stop after three years or four. They can’t be there forever. So some of those patients get excluded. So those studies really are not valid.” He added, “Disease-free survival is still worth it. If you are living for 100 years, whether you live with disease or without disease, but if you’re still alive, that counts, right?”
(I’ve written about overall survival versus disease-free survival here. Specifically, “If cancer is going to recur – and that’s a big ‘if’ – endocrine therapy can most likely delay that recurrence, but it can’t prevent it. Still, that delay has its uses. The earlier that recurrence happens if it’s going to happen, the more tests and treatments one undergoes. Endocrine therapy can thus conceivably reduce the number of procedures involved. That’s not chump change.”)
I told my oncologist, “I know that the disease-free survival is extremely important and really not looked at often enough, because it makes a difference in terms of treatment, collateral damage, financial toxicity.”
He said, “Even for patients it makes a difference. If they are living without disease, that’s still pretty good. Those are some of the academic arguments they always have, but in the field practically, we have to make sure that we meet the expectation of the patient and not some professor sitting somewhere who never sees patients. And has no patients sitting across the table like this, asking questions.”
He added, “Guidelines are only guidelines. They’re not like the Ten Commandments. We follow the guidelines where we feel it’s necessary. But in the field, supposing we didn’t do anything and there is a recurrence two years down the line? They will say, ‘How come you didn’t do anything? You didn’t do any scan, you didn’t do any markers. How can we know?’ Sometimes patients have asymptomatic metastases. In the lymph node or liver or lungs, somewhere. It doesn’t cause any problem. If you feel a small lump in the breast and that doesn’t bother you, that doesn’t mean you shouldn’t recognize it.”
(In fact, I had been asymptomatic for years, not even feeling my 1.8-cm. tumor during self-exams because it was located so close to muscle. My tumor had stood out on mammograms like a sore thumb, but was so slow-growing that it had been graded repeatedly as benign.)
My oncologist concluded, “Guidelines, they are studying to reflect populations, not individual patients. The individual patient may go up or down, but they are looking at bulk. The good news is you are normal, and I will see you in three months.”




GypsyWynd ⋅ May 21, 2017
Glad there was good news in the end.
ConnieK ⋅ May 22, 2017
CONGRATS for the good news!!!!!
TruNorth ⋅ May 22, 2017
Nice to see the good news.