Variables in Here Be Dust
- Feb. 3, 2016, 3:51 p.m.
- |
- Public
One of the advantages of posing the same question to different doctors on my medical team is that I get to peek through their respective lenses. (My lens is that of a layperson, so I present my doctors’ info as I best understand it. Any errors in interpretation are my own.)
My surgeon, the last team member on my post-hospitalization doctor dance card, said that my blood clot arising from my port occurs in about 2-3 percent of cases. He doesn’t think the anastrazole played a role, despite its small chance (as with any endocrine therapy) of causing a clot. There is always some clotting that occurs around a port catheter, he said. Mine happened to have gotten out of hand. My surgeon is on Team Anastrazole.
My radiation oncologist is not that impressed by endocrine therapy to begin with. True, it’s been shown to improve disease-free survival, he said; but the studies he’s seen show no difference in overall survival. If cancer is going to recur – and that’s a big “if” – endocrine therapy can most likely delay that recurrence, but it can’t prevent it. Still, that delay has its uses. The earlier that recurrence happens if it’s going to happen, the more tests and treatments one undergoes. Endocrine therapy can thus conceivably reduce the number of procedures involved. That’s not chump change.
I asked him (along with my surgeon) about tumor heterogeneity. My Oncotype-DX score was intermediate (22), which is why I had undergone chemo. With luck, I am rid of all cancer cells, but nothing is guaranteed. If any undetectable cells remain, they can potentially mutate, and there’s a chance that endocrine therapy itself might predispose those cancer cells to do just that.
My radiation oncologist explained that sometimes it’s better to not get rid of some cancer cells, because they compete for resources in the body. Starving out a class of cancer cells removes competition, creating the potential (even if small) for other cancer cells – say, those with a different genome, unaffected by endocrine therapy – to strengthen.
I said that to me, that sounds analogous to the way bacteria function. He agreed.
So, I have variables to weigh, and a lot of unknowns.
If I assume that a recurrence can happen – if it’s a “pay now or pay later” proposition – I want to push it back if I can. The number bandied about is that about 30% of breast cancer patients metastasize, but that number itself is suspect. (See also here for even more nuance; free registration is required to view).
As I perceive their reactions, my medical oncologist (MO) places less weight than my radiation oncologist (RO) does on the finding that, in the long run, the recurrence rate is higher for those with ER-positive cancers (which mine was) than for those with ER-negative cancers (ER = estrogen receptor). My MO views those percentages as being too small to begin with. I don’t think my RO views those percentages as any great threat, either, but he acknowledges that they exist. Early on, ER-positive patients have a lower risk of recurrence than ER-negative patients do, but the percentages during that earlier period are higher all around – hence the use of endocrine therapy for ER-positive patients.
Also, recurrence doesn’t necessarily mean metastasis. As explained in the American Journal of Managed Care, “Patients with hormone receptor–positive tumors have a recurrence rate that is twice as high as those with hormone receptor–negative tumors at 5 years posttreatment. Women with ER-positive tumors have a greater risk of recurrence in later years than in the first 2 years. Overall, ER-positive tumors are associated with a long-term recurrence rate of 2% per year but are less likely to cause death from breast cancer than other tumor subtypes. Overall, patients with hormone receptor-positive tumors have the best outcomes.”
Currently, the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program (SEER) does not track which breast cancer patients metastasize, but counts only those patients who had been initially diagnosed with metastasis, i.e., de novo. (This is one reason why efforts like The MBC Project – which is working to fill that information gap – are crucially important.)
So, my chance of recurrence/metastasis versus the risk of another blood clot is one variable for me to consider – and, within that, the timing of potential recurrence. That timing also considers the frequency and cost of potential procedures, which can then involve the prospect of financial toxicity and quality-of-life issues. Against that, I am weighing other QoL issues, mainly with respect to side effects from the anastrazole. The questions I consider are:
-
What do I think my chances are of developing a blood clot if I continue to take anastrazole? (Theoretically they’re low, but my MO seems more concerned about this than my surgeon. My RO seems to fall in-between the two. I feel more in sync with my surgeon on this, but we all agree that a second clot – especially now with my port gone – would mean an end to endocrine therapy for me.)
-
How important is anastrazole to me for trying to prevent recurrence? (My surgeon seems to give more weight to this than either my MO or my RO. My MO factors it into his concern about my blood clot. My RO gives less weight to endocrine therapy with respect to overall survival, but acknowledges its value in prolonging disease-free survival. I place a high value on DFS.)
-
How do I weigh (1) and (2) against my current quality of life? (My side effects – mainly exacerbation of my carpal tunnel syndrome – are currently manageable, and I am monitoring my bone health. Under ordinary circumstances I would engage in my usual weight-bearing exercise. Current precautions to take with my blood clot-swollen right arm means I have to lay off lifting my weighted vest for a while.)
-
Does the blood clot affect how I view potential long-term risks of anastrazole? (Not really. Those risks remain the same, and I weigh them against (1) and (2).)
So, for now (important qualifier), I’m still on Team Anastrazole.
Not having my port anymore feels strange. That area near my clavicle is mostly flat again, with just a bit of swelling as my deja-vu scar heals behind surgical skin. Deja-vu because I’d had a similar (though more extreme) scar after my port had been inserted, before it had healed into a thin line. That small dome beneath my skin and the line into my jugular had become part of my transformed body, alas with serious consequences. Once again I am left at the mercy of my cantankerous veins for blood draws, but my wistfulness is about more than that.
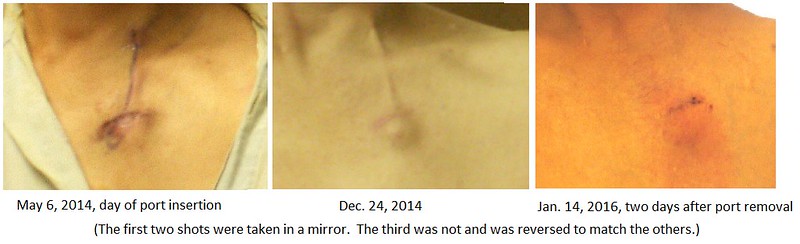
In a sense, the port removal reverts my upper chest to a visual “before” state, which is a lie. I am no longer that person. Aside from its convenience, my port had been a testament to the bizarre turn that my life had taken. It helped to tell my story, acting as a kind of visual shorthand, and in that way it had become part of my identity. I find myself having to adjust to its absence.
Last week I called the Xarelto CarePath Support Program after their literature arrived in the mail. I was still waiting for my savings card (now received), which will cover the cost of the blood thinner.
Good thing I called. Their rep told me that the program allows for only one refill every 30 days. Typically one would take a 15-mg pill twice a day for 21 days and then switch to a 20-mg pill once a day. In my case, I’m taking the 2x15-mg pills for six weeks before I make the switch.
If I refilled the 15-mg prescription to take me through the six weeks, the savings program would not cover the cost of the 20-mg prescription because I would be filling it too soon (after about two weeks rather than after 30 days).
The rep said I could get around that limitation by getting a starter pack of the 15-mg from my PCP, which would complete the six weeks once I finish my initial 30-day prescription. I dashed off a memo to that effect and dropped it off at my PCP’s office on my way to the appointment with my surgeon. This week I picked up the pills to tide me over. That teaches me that double-checking with a patient support program is always a good idea.
I also called my insurer, which is straightening out the claim for my hospitalization. It should take about a month for the corrections to show up, at which time I’ll have the needed paperwork to obtain a refund from the hospital.
“Side by Side” incorporates stencils from Beeton’s Book of Needlework and Batik and Other Pattern Dyeing, along with astronomical star stencils.
“Spirit World” uses stencils (all considerably color-altered) made from William Swainson’s Zoological Illustrations, New York Public Library Digital Collections, Farm Security Administration Photographs, The Brochure Series of Architectural Illustration, Beeton’s Book of Needlework, the treeline from one of my photos (similar to this shot), and a magnified image (made with my Plugable USB microscope) of blood on gauze, from my recent, post-port removal, failed blood draw attempts.




GypsyWynd ⋅ February 03, 2016
That is a lot of information to digest and consider.
Deleted user ⋅ February 11, 2016
I love reading about your life. I see the words "strength" and "courage" written between the lines. :-)